
Комплексний посібник з розробки та обслуговування програмного забезпечення для управління автопарком
Готове програмне забезпечення для управління автопарком не було розроблено для вашого автопарку. Воно було створено для всіх — і це саме проблема.

Комплексний посібник з розробки та обслуговування програмного забезпечення для управління автопарком
Готове програмне забезпечення для управління автопарком не було розроблено для вашого автопарку. Воно було створено для всіх — і це саме проблема.

Розробка застосунку для таксі: етапи, функції, вартість і помилки
Коли InDrive вийшов на ринок, здавалося, що після Uber, Bolt і Lyft на ньому не залишилося місця. Але завдяки чіткій бізнес-моделі та сфокусованому, гнучкому продукту компанія зайняла свою нішу і масштабувалася.

5 найкращих програм для диспетчеризації вантажних перевезень
Протягом останніх років галузь вантажоперевезень зіткнулася з численними викликами. Від пандемії COVID-19 та пов'язаних з нею обмежень через зменшення обсягів перевезень і зниження тарифів

Топ-7 систем управління транспортом у 2025
Незалежно від того, наскільки великий ваш бізнес і як довго ви працюєте на ринку, рік за роком ви будете задавати собі одні й ті ж питання, як і кожен власник бізнесу.

10 найпоширеніших ризиків у ланцюгах поставок і як їх уникнути
З 2026 роком на горизонті, геополітика є найбільшим загрозою для глобальних ланцюгів поставок. Війни та політична нестабільність порушують торгові маршрути та ускладнюють логістику по всьому світу.

Покроковий гайд із розробки додатку для доставки посилок на вимогу
Дуже важливо подумати про те, як розробити рішення для задоволення потреб користувачів, залишаючись конкурентоспроможним на ринку, коли ви плануєте створити додаток для доставки посилок.
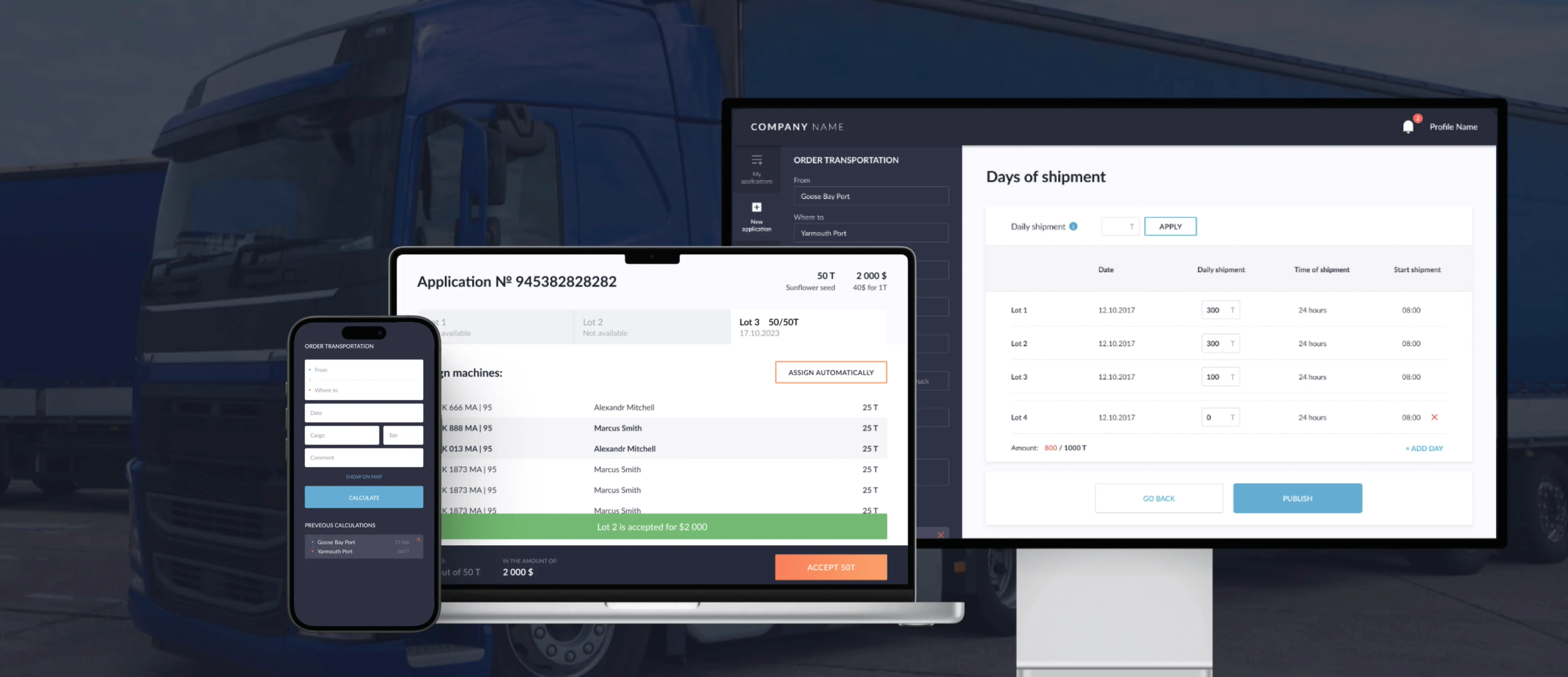
Як створити кастомізовану TMS систему для оптимізації логістики: процеси, етапи
Готові платформи TMS часто обіцяють гнучкість, але спробуйте адаптувати їх до вашого бізнесу, і ви швидко зіткнетеся з труднощами. Диспетчери знаходять обхідні шляхи.
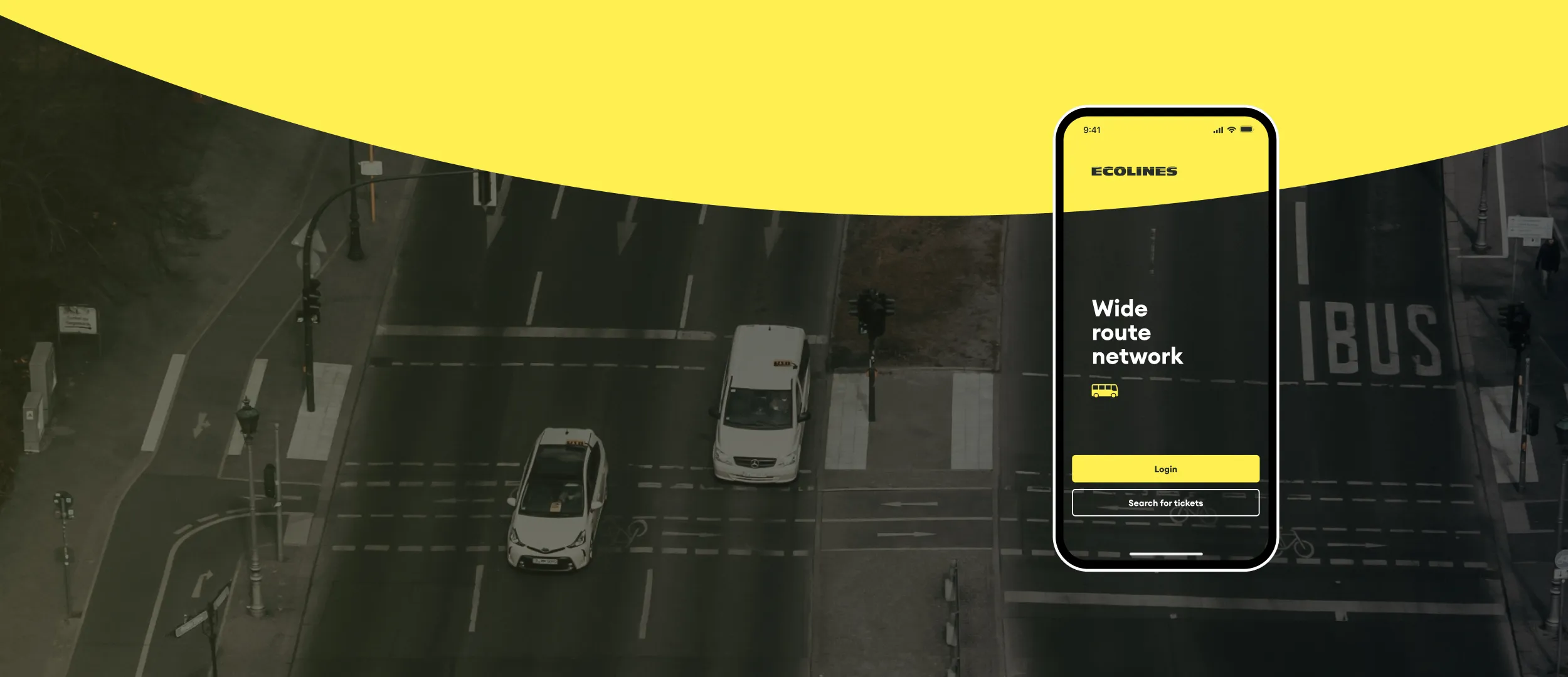
Мандрівники ненавидять стояти в чергах або мати справу з паперовими квитками. Незалежно від того, чи це літак, потяг або автобус, люди очікують, що зможуть забронювати квитки кількома дотиками на своєму телефоні.

Платформа райдшерингу: розробка, функції та вартість
Райдшеринг у 2026 році — це вже не експеримент, а частина міської транспортної інфраструктури. За оцінками Mordor Intelligence, сегмент shared mobility зростає приблизно на ~17% CAGR до 2031 року.

Як створити індивідуальну систему управління замовленнями (OMS): витрати, етапи та функції
Розглядаєте можливість створення системи управління замовленнями (OMS)? Тоді ви, напевно, знаєте, що є два варіанти: купити готове рішення (корпоративні варіанти, такі як IBM Sterling OMS, або ніші, такі як Zoho Inventory)

Розробка ERP-системи: як створити кастомну ERP для бізнесу
За останні роки ERP стала базовою системою управління бізнесом — але у 2026 компанії очікують від неї не лише обліку, а гнучкості, швидких змін процесів, інтеграцій, аналітики в реальному часі та безпеки даних.

Розробка MVP для стартапів: Чому вашому стартапу потрібен MVP?
Dropbox запустився з простого пояснювального відео. Airbnb почав із здачі в оренду надувного матраца. Це були не щасливі випадковості — це були розумно створені MVP.

Система управління запасами на виробництві: як побудувати та автоматизувати
У виробництві система управління запасами — це інструмент, який тримає під контролем матеріали, комплектуючі й готову продукцію, щоб уникати простоїв, термінових закупівель і перевантажених складів.

Моноліт vs мікросервіси: яку архітектуру обрати для вашого продукту
Розробники програмного забезпечення часто дискутують, чи варто використовувати монолітні архітектури чи мікросервіси. Вибір правильних архітектурних патернів є вирішальним для створення масштабованих, підтримуваних і ефективних програмних систем.

Інхаус розробка vs аутсорсинг: що обрати бізнесу
Кожен рік технологічний світ стає складнішим, а потреби великих компаній постійно зростають. Деякі бізнеси вирішують встигати за інноваціями, розбудовуючи власні команди розробників, тоді як інші звертаються до аутсорсингу розробки.
Допомагаємо транспортним і логістичним компаніям масштабуватися швидше: